Stargardt’s disease is a rare eye condition that affects both children and adults, in many cases leading to blindness. It has several different varieties, and new research indicates that each requires a slightly different therapeutic approach. This key discovery may contribute to the development of effective methods to combat this currently incurable disease.
Initially, patients experience a sudden loss of sharp and central vision. The disorders progress, often making normal functioning difficult, including reading or face recognition. For many people, just looking at a light source is painful. After some time, the disease may stabilize, but often the damage to the macula is so significant that vision loss occurs.
The above description concerns Stargardt’s disease, a disorder that affects approximately 1 in 10,000 people, most often children between 8 and 12 years of age. There is no cure for this macular dystrophy, but understanding the mechanisms that occur in photoreceptors during the disease is crucial for potential therapeutic interventions (several drugs are being tested). It turns out that different types of Stargardt’s disease – although they have a similar cause – respond differently to different classes of drugs.
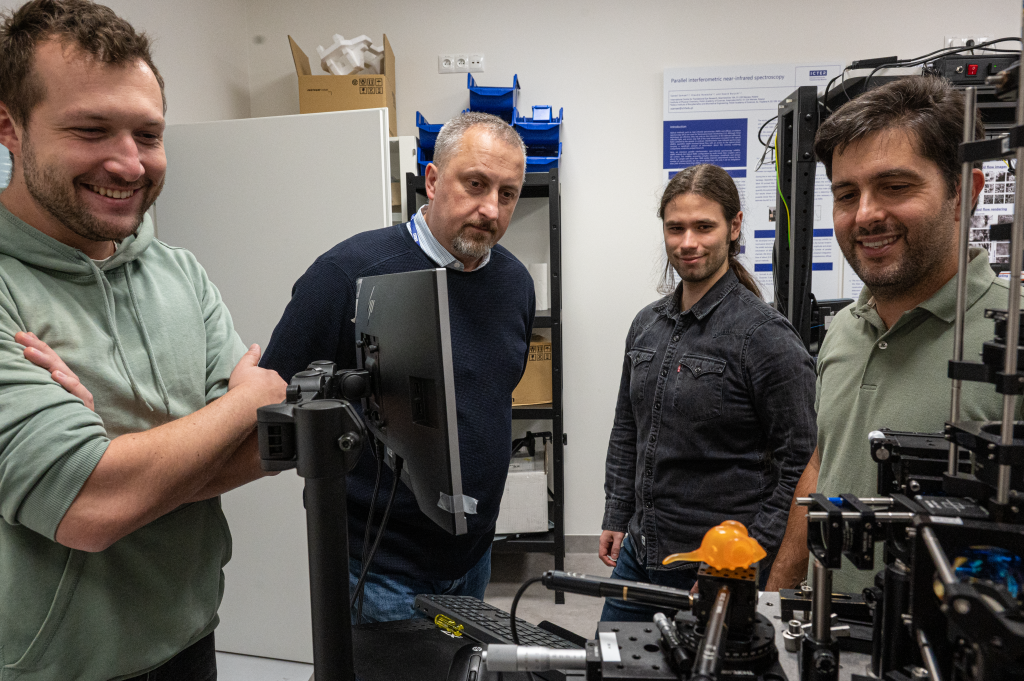
Research conducted with the participation of scientists from the International Centre for Translational Eye Research (ICTER) at the Institute of Physical Chemistry, Polish Academy of Sciences, including Dr. Marcin Tabaka, Dr. Andrzej Foik, Dr. Damian Panas, Dr. Jagoda Płaczkiewicz, and Dr. Katarzyna Kordecka, in cooperation with the Center for Translational Vision Research at the Gavin Herbert Eye Institute (CTVR) from UC Irvine in California under the supervision of Prof. Krzysztof Palczewski, resulted in a paper published in PNAS entitled “Distinct mouse models of Stargardt disease display differences in pharmacological targeting of ceramides and inflammatory responses”, which increases our understanding of Stargardt’s disease.
Stargardt’s disease is not just one disease
Lipids are an important component of the biological activity and physiology of most cells in the body, and in particular, they play a key role in the functioning of the retina. It has been confirmed that disturbed lipid homeostasis occurs in various degenerative retinal diseases, although still little is known about lipid profiles in normal and diseased retinas.
Stargardt’s disease is characterized by the accumulation of a non-degradable derivative of the visual pigment – lipofuscin – in the retinal pigment epithelium (RPE), which causes its atrophy. From the first description of Stargardt’s disease until recently, its diagnosis was based on the evaluation of the phenotype by eye examination, but since the advent of genetic testing, the picture of the condition has become more complete.
What was originally thought to be one disease is probably at least three variants (STGD1, STGD4, STGD3), each associated with a different genetic change. Therefore, it is extremely difficult to clearly define what Stargardt’s disease is, let alone think about potential treatments.
The most common form of Stargardt disease – STGD1 – is caused by biallelic variants of the Abca4 gene (i.e. autosomal recessive), and their exact genotype (i.e. combinations of both variants) is of great prognostic importance as to the age of disease onset and its progression. The frequency of Abca4 allele carriers in the general population is 5-10%, and different gene combinations influence the age of onset and the severity of the disease itself. Furthermore, disease severity is inversely related to ABCA4 function, and mutations in this gene are thought to play a role in other diseases such as retinitis pigmentosa, rod and cone dystrophies, and Age-Related Macular Degeneration (AMD). Macular Degeneration).
Biochemistry of Stargardt’s disease
Two genes encoding lipid-processing proteins have been associated with inherited retinal degenerative diseases. Mutations in the gene encoding an enzyme called ELOVL4 elongase, involved in building long-chain fatty acids, have been associated with autosomal dominant AMD-like Stargardt disease – STDG3 variant. Patients suffering from this disease at a young age experience loss of central vision. In turn, the disease in people suffering from STGD4 has been associated with mutations in the Prom1 gene. This disease variant was discovered in 1999 and little is known about its cause, except that there is a mutation at the p.R373C site, which causes dystrophy of cones and rods.
However, the most common form of Stargardt disease – STDG1 – is quite well understood. Patients showed a progressive bilateral appearance of yellow-orange spots (lipofuscin) in the macula, where the density of cones is highest. Such changes cause atrophy of the RPE and the death of photoreceptors in this region, resulting in vision loss. Lipofuscin accumulation in the RPE is a characteristic finding in the eyes of STGD1 patients and the mouse model of Stargardt disease.
Previous studies have shown that ABCA4 is expressed in the photoreceptor outer segment disc (POS disc) and the plasma membrane of RPE cells. ABCA4 transports a retinal phospholipid compound known as N-retinylidene-phosphatidylethanolamine (N-ret-PE) upon photoexcitation, allowing its removal from receptor cells – similarly to RPE cells, where N-ret-PE is transferred to lysosomes or phagosomes. In people with Stargardt disease (STDG1), N-ret-PE accumulates in POS discs and leads to the formation of the precursor A2E bisretinoid (A2PE). Inside the RPE lysosomes, A2PE is converted into A2E – a compound that cannot be broken down by any enzymes in the body. A2E is believed to react with other lipids and convert to lipofuscin deposits.
According to the current knowledge, over 100 mutations affect ABCA4 functions and are associated with a wide spectrum of Stargardt disease phenotypes. The suggestion that mutations in different domains of ABCA4 may affect the RPE and photoreceptors differently is tempting, meaning that ABCA4 has slightly different functions in them. This, in turn, opens a window into the potential therapeutic mechanism associated with lipid-lowering drugs.
Therapeutic hopes
Although there is no cure for Stargardt’s disease, work is underway on several therapies aimed at limiting or completely stopping the progression of this disease. The team led by Prof. Palczewski at CTVR and ICTER decided to investigate two alternative mouse models of functional ABCA4 deficiency to model the heterogeneity of mutations in patients with Stargardt disease and to see whether a different therapeutic approach might be necessary to stabilize retinal health in each case.
Using a combination of molecular techniques, the researchers examined Abca4 knockout mice (knock-out) and mice with additional Abca4 (knock-in). The researchers compared the two strains to determine whether they exhibited differential responses to factors that affect cytokine signaling and/or ceramide metabolism, as changes in either of these pathways can exacerbate retinal degenerative phenotypes.
Abca4 knockout and Abca4PV/PV knockout mice showed different responses to a ceramide-lowering drug and an immunomodulatory drug. The two mouse models were found to have divergent levels of baseline cellular stress and signaling, which are exacerbated in the early stages of light-induced retinal degeneration. Most importantly, these side effects can be alleviated prophylactically with the use of an immunomodulatory drug, thus “slowing down” the course of Stargardt’s disease.
“We found varying degrees of response to maraviroc, a known immunomodulatory CCR5 antagonist, and to the ceramide-lowering agent AdipoRon, an agonist of ADIPOR1 and ADIPOR2 receptors. Our phenotypic comparison of two different mouse models with the Abca4 mutation sheds light on potential therapeutic options previously unexplored in the treatment of Stargardt’s disease and provides a substitute test for assessing the effectiveness of gene therapy” – says Dr. Marcin Tabaka, leader of the ICTER Computational Genomics Team.
It is worth mentioning that in an earlier study, also published in PNAS, entitled “Stress resilience-enhancing drugs preserve tissue structure and function in degenerating retina via phosphodiesterase inhibition”, molecules that activate biological mechanisms of stress resistance were examined. This, in turn, may result in the development of a new class of pharmaceuticals, the so-called drugs that increase stress resistance (SRED) with potentially wide clinical significance for combating pathological retinal changes, not only Stargardt’s disease. A major contribution to the research work was made by the ICTER Computational Genomics Team, which analyzed single-cell sequencing data, enabling the identification of universal molecular mechanisms involved in age-related eye diseases and hereditary retinal degenerations.
The latest study makes a case for using transgenic knock-in mouse lines that have mutations analogous to those in humans. It also serves as a precursor to adopting these models to test genome editing methods that can precisely correct genetic mutations. Thanks to these efforts, Stargardt’s disease, which is today considered “incurable”, may become a disease that can be controlled and, as a result, save eyesight.
Author of the press release: Marcin Powęska.
Image: Deposit Photos.
Cited papers:
https://doi.org/10.1073/pnas.2314698120
https://doi.org/10.1073/pnas.2221045120